4 min|Rhiannon Lockhart
Understanding PCOS: Symptoms, Causes, and Management
Pelvic Restoration, Sexual Health, Hormones, FertilityPolycystic Ovarian Syndrome (PCOS) is a hormonal condition that can manifest at any point after the onset of menstruation. Its symptoms can fluctuate over time and may be influenced by factors such as diet, stress, and lifestyle. Shockingly, PCOS affects nearly 1 in 10 females of reproductive age, yet up to 70 percent of those with PCOS remain undiagnosed worldwide. (1)
Common PCOS Symptoms
The symptoms of PCOS can vary widely from person to person but typically include:
Hirsutism (male-pattern hair growth) or male-pattern hair loss
Anovulatory cycles
Weight gain, especially around the midsection
Insulin resistance
Enlarged ovaries or polycystic ovaries
Skin tags
Infertility
To receive a formal diagnosis, individuals must meet at least two of the following criteria:
1. Irregular, heavy, or missed periods due to anovulatory cycles (missed ovulation).
2. Signs of elevated androgen (male hormone) levels, confirmed through blood tests.
3. Presence of ovarian cysts.

Exploring the Root Causes of PCOS
Although the precise cause of PCOS remains elusive, several factors play a role, including genetics, insulin resistance, and androgens. (2)
To better understand PCOS, let's briefly delve into the world of hormones.
The ovaries play a pivotal role in hormone production, particularly estrogen and androgens. Androgens, often associated with "male hormones," are more predominant in male bodies. However, individuals with PCOS experience an imbalance between "male" and "female" hormones, featuring higher-than-normal androgen levels.
Many PCOS symptoms stem from issues with insulin, primarily insulin resistance. Those diagnosed with PCOS often face a higher risk of prediabetes and type 2 diabetes. Excess insulin can also contribute to increased androgen production.
Nutritional Strategies for Managing PCOS
Dietary changes should be among the first strategies considered for PCOS management since insulin resistance can be addressed with the right diet. Here are some general dietary guidelines:
Prioritize a diet that regulates blood sugar levels. The level of strictness should align with your degree of insulin resistance. Continuous glucose monitoring can provide insights into your body's carbohydrate responses.
If you have high insulin resistance, consider a low-carb diet until your blood sugar levels stabilize.
Always combine carbohydrates with protein and/or healthy fats.
Opt for "slow" carbs with higher fiber content, such as beans, legumes, squash, parsnips, oats, quinoa, and brown rice, as they have a milder impact on blood glucose levels.
Aim for 20-30g of protein per meal.
Include anti-inflammatory foods like fatty fish, olive oil, green tea, leafy greens, cruciferous vegetables, and berries.
Reduce dairy intake, as it can exacerbate symptoms of androgen excess, such as acne.
Eliminate alcohol from your diet, as it can disrupt hormone balance and affect blood glucose levels, especially when consuming beer, wine, or sugary cocktails.
Reduce or eliminate caffeine, as it can raise blood sugar levels and disrupt hormones. If you need caffeine, consume it after breakfast.
Avoid processed foods, fried items, packaged snacks, sugary drinks, refined flours, and white bread.
Never skip meals.
Lifestyle Recommendations for PCOS
In addition to dietary changes, consider the following lifestyle adjustments:
Exercise regularly to increase insulin sensitivity and manage weight. Strength training and aerobic exercises are particularly beneficial for PCOS.
Manage stress effectively, as many PCOS cases involve adrenal components that stress can exacerbate.
Establish a consistent sleep schedule, aiming for 7-9 hours of quality sleep each night.
Consult with your healthcare provider to determine suitable supplements for managing PCOS.
Potential Complications of PCOS
While PCOS can lead to various complications, lifestyle changes, dietary adjustments, and supplements can help mitigate these risks. Collaborate with your healthcare provider to create a tailored plan.
Infertility: Approximately 50 percent of individuals with PCOS report primary infertility. Contributing factors may include insulin resistance, associated weight gain, endometrial abnormalities affecting implantation, and changes in ovarian function. (3)
Metabolic Risks: Weight gain and PCOS often share a bidirectional relationship due to blood sugar issues. Insulin resistance, prevalent in PCOS, increases the risk of developing type 2 diabetes when not managed early. (3)
Cardiovascular Health: PCOS is linked to an increased prevalence of risk factors for cardiovascular disease. Conditions associated with metabolic syndrome and inflammation are common among those with PCOS, raising the risk of long-term complications. (4)
Understanding and managing PCOS involves a holistic approach that combines medical care, dietary adjustments, and lifestyle changes. Collaborate closely with your practitioner to navigate the complexities of PCOS and work toward a healthier future.
Are you looking for support with improving your health and longevity?
Click here to book a consultation with one of our experienced Practitioners today!
Related Articles
4 min|Dr. Alex Chan
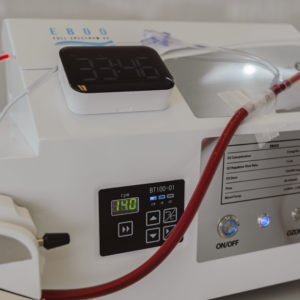
EBOO for Chronic Inflammation: A Natural Approach for Systemic Relief
Regenerative Medicine, EBOO Therapy
4 min|Dr. Alex Chan
EBOO Therapy for Autoimmune Conditions: Exploring the Potential Benefits
Autoimmune Disease, Regenerative Medicine, EBOO Therapy


