5 min|Integrative
The Gut-Brain Connection
Wellness, Mind Health, Health, Gut HealthThe Gut-Brain Axis: How Our Gut Affects Our Brain & Vice Versa
The gut-brain axis refers to a bidirectional communication system between the central nervous system, including the brain and spinal chord, and the digestive tract. Due to this complex communication system, our cognitive and emotional responses can influence our gut.
Recently, we have begun to understand that this relationship also allows for communication from the gut to the brain, enabling gut health - or dysfunction - to influence brain health. (1)
"I've got a gut feeling about this"
"There are butterflies in my stomach"
"I feel gutted about this"
Brain to Gut
Our language reflects the connection between our brain and our gut. When we feel uneasy about something, we might feel it within our digestive system; alternatively, when we’re sure, we feel rock solid in our gut. This is due to the strong nervous system connection between the brain and gut.
It is due to this connection that thinking about food, or smelling food, triggers a release of stomach acid and digestive enzymes, in preparation for digestion. It also means that when we are stressed, our ability to digest food is compromised. The vagus nerve, a nerve that connects the brain stem to the thoracic and abdominal cavities, plays a key role in this communication.
The vagus nerve is the main nerve of a branch of the nervous system known as the parasympathetic system. The parasympathetic nervous system helps us to rest, relax, and digest. The vagus nerve carries out its messages, causing our heart rate to decrease, respiration rate to lower, and gut motility and release of bile, enzymes, and stomach acid, to increase.
Alternatively, when we are stressed, this communication decreases, and our heart rate increases, breathing rate increases, and ability to digest is compromised. Due to this strong connection, how our brain feels about our current situation (ie. whether we feel stressed or blessed), determines how the rest of our body, including our gut, is functioning.
Gut to Brain
The vagus nerve carries information from the brain to the gut, affecting digestion and absorption. But this pathway is a two-way street; the vagus nerve also carries information from the gut up to the brain(2). In fact, 80-90% of the fibers of the vagus nerve carry information from the gut to the brain. These fibers play a large role in regulating the hypothalamic pituitary and adrenal (HPA) pathway, a hormone pathway with many functions, including stress signaling(3,4).
We are beginning to understand that this communication is highly influenced by bacteria, fungus, and viral activity in the gut, collectively known as the microbiome. By way of the vagus nerve, the microbiome can influence activity of the brain(5). Due to this connection, it appears that detrimental changes to the gut microbiome may be associated with the etiology of a variety of psychological and neurological concerns.

Heal the Gut, Heal the Brain
You may have heard of ‘leaky gut’, also known as increased intestinal permeability. Leaky gut occurs when inflammation creates small holes in the gut lining, compromising the integrity of it, and allowing particles of food, toxins, and microbes into the blood stream. It is an issue that has been linked to a variety of health conditions (Leaky Gut).
At the root of this issue is zonulin, a regulator of tight junctions, the doorways of the gut lining; in a healthy gut, the tight junctions are highly regulated, trafficking specific macromolecules in and out the bloodstream. In an inflamed gut, zonulin is affected, and the gut lining becomes dysregulated and ‘leaky'. The gut microbiome plays a large role in modulating inflammation in the gut and helping to maintain integrity of the gut lining(6).
This integrity influences the immune system, and the balance between mounting a response to outside threats and tolerating, and protecting, our own tissue(7). Many structural similarities exist between the gut lining and the lining between blood vessels and the brain, also known as the blood brain barrier (BBB).
Recent evidence indicates that the BBB is susceptible to changes in the gut lining and gut microbiota(8). Via these mechanisms, inflammation in the gut may directly affect the integrity of the BBB. Changes in the gut microbiome have been associated with conditions previously thought of as brain concerns, such as depression, anxiety, and Alzheimer’s disease(9,10). It is suspected that the microbiome communicates with the brain via complex mechanisms of the nervous, endocrine, and immune systems.
Recent research shows direct movement of a protein associated with Parkinson’s travelling from the gastrointestinal tract to the brain, via the vagus nerve, illustrating that the vagus nerve may act as a direct conduit for material from the gut to the brain.(11)
Takeaway
Extensive research has shown that a healthy vagus nerve communicates from the brain to gut, as well as from the gut to the brain. It follows that a dysfunctional gut would lead to a dysfunctional brain, due to this complex bi-directional pathway.
In order to heal the brain, first, we must heal the gut.
REFERENCES
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
- Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ. Nerves and Nerve Injuries: Vol 1: History, Embryology, Anatomy, Imaging, and Diagnostics. Cambridge, Massachusetts: Academic Press (2015).
- https://link.springer.com/article/10.1007%2Fs40473-014-0010-5
- https://link.springer.com/article/10.1007%2Fs00335-013-9488-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
- https://www.nature.com/articles/cmi201067
- https://www.nature.com/articles/ncpgasthep0259
- https://www.frontiersin.org/articles/10.3389/fncel.2015.00392/full
- https://www.ncbi.nlm.nih.gov/pubmed/29134359
- https://www.nature.com/articles/s41598-017-13601-y
- https://www.ncbi.nlm.nih.gov/pubmed/25296989?dopt=Abstract
Related Articles
5 min|Dr. Alex Chan
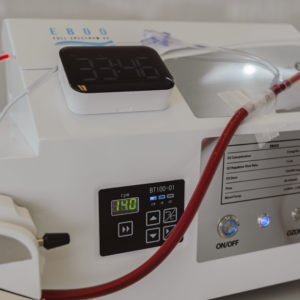
EBOO for Chronic Inflammation: A Natural Approach for Systemic Relief
Regenerative Medicine, EBOO Therapy
5 min|Dr. Alex Chan
EBOO Therapy for Autoimmune Conditions: Exploring the Potential Benefits
Autoimmune Disease, Regenerative Medicine, EBOO Therapy


